A Thorough Debunking of COVID-19 Contrarianism
Data scientist Jennifer Handsel deconstructs the truth and the myths of COVID-19.
The COVID-19 pandemic has proven a challenge to governments worldwide, and liberal democracies in particular have struggled to both contain the virus and keep citizens informed of the dangers. Within this context, a particular brand of political rhetoric has emerged: President Trump has unfavorably compared the risks to car crashes, Boris Johnson has appealed to “British common sense,” and a former U.K. Supreme Court justice has stated that we are suffering from “collective hysteria.” If only we could go back to a time when reason prevailed, we would—these men suggest—see that our response to the pandemic has been far too extreme.
This blasé attitude has had disastrous consequences. Johnson came down with COVID-19 after continuing to meet members of the public and shaking hands with everyone, including sick hospital patients. He had to be hospitalized, and only recovered after receiving intensive care—at a time when ordinary citizens were being turned away from hospitals. Trump (and much of his entourage) became sick after holding numerous political rallies, but also recovered after treatment with a risky corticosteroid and an experimental antibody unavailable to the general public.
But despite the high infection rate even among the most powerful people in the world, and 1.11 million deaths and counting worldwide, COVID skepticism is still a popular pastime. The most prolific of the COVID skeptics, and probably the best regarded, is Alex Berenson, formerly of the New York Times. Berenson started his career as a business journalist, most notably publishing a book which analyzed the trend towards corporate mismanagement that led to the Enron scandal. He later spent time in Iraq as a war correspondent, and after leaving journalism became an award-winning fiction author. In 2019, he gained widespread media coverage with Tell Your Children, an intensively researched nonfiction book which argues that marijuana is far more harmful than commonly understood.
Over the past year, Berenson has found new notoriety by arguing that COVID-19 is far less harmful than experts would have you believe, and that lockdowns are in fact the greater harm. He is prolific on social media, having gained 200,000 followers on Twitter, but is also taken seriously in much wider circles. In recent months, Berenson has given numerous interviews on Fox News, and authored several opinion pieces in the New York Post, each time arguing against lockdowns. He’s even gone so far as to publish his argument in a “book,” which is really more of a pamphlet: Unreported Truths about COVID-19 and Lockdowns: Part 1. (He has already released a part 2.) Rather than dismiss his arguments offhand, I think it’s important to examine the main claims Berenson makes in Part 1 of his book, and in doing so attempt to explain, in layman’s terms, what we know about the virus, how we know it, and why Berenson’s arguments are so misplaced and dangerous.
Berenson’s claims can be roughly divided into two categories; first, that the coronavirus is not as bad as people think, and second, that the measures recommended by experts do not work. In both cases, Berenson’s conclusion is clear: do not trust the experts. But let’s dive in.
A. “Coronavirus is not that bad”
The principal thesis of Unreported Truths is that we have vastly overestimated the dangers of the pandemic, and the measures that we have taken have caused great harm:
By mid-April, it was obvious to me that the coronavirus epidemic simply was not going to be anywhere near as bad as the early predictions, and that the lockdowns were an extreme overreaction.
…
So, yes, the coronavirus epidemic has largely ended as a medical crisis. But for now, the policies it has spawned remain educational, economic, and societal millstones.
The book aims to explain to the reader how Berenson came to this conclusion, with reference to scientific evidence:
I will provide links to the papers and data I reference so you can judge whether the sourcing backs my answers. I am committed to following the truth and offering the most honest answers, whatever they may be.
In these times of uncertainty and misinformation, Berenson’s aim appears laudable. We sorely lack charismatic communicators who understand the science and are able to keep the general public informed. So what does he have to say?
1. The virus only kills old people, thus it is not ‘really deadly’
Berenson starts his book with the observation that COVID-19 is far more likely to kill people over 80 than under 50. As a scientific claim, this is undisputed, and for the record I reproduce the table he cites below.

From this, Berenson concludes that the coronavirus cannot really be considered “deadly”:
I knew coronavirus was more dangerous to older people, of course—but I assumed young people would also face serious risks. After all, any really deadly virus could hardly spare the young or middle-aged.
Although technically based on scientific data, this is actually a moral argument: the virus only kills a certain segment of the population, so it’s not really a threat to the rest. The implication is that the life of this segment of the population has less value than that of other segments of the population. Indeed, Berenson makes this claim directly:
Who would disagree that the death of a 10-year-old is harder to accept than, say, an 88-year-old? The child is only beginning her life; the man has already had his.
It is for the reader to decide whether to accept this value claim or not, but I for one would be incredibly upset if one of the elder members of my family, who still have a decent life expectancy and a well-earned retirement to enjoy, were to suddenly die. I do not believe that I would stoically dismiss their passing by saying “Well! They were old.”
While we’re on the subject of moral values, an almost universal value is that preventable deaths are a very bad thing, precisely because they are preventable. I think that we can all agree to the principle that behaving in a way that puts others in danger is unacceptable, and that we have a moral obligation to help those in need—and we can therefore agree that it is morally appropriate to change our behavior to protect those vulnerable to COVID-19.
And the dangers posed by the coronavirus cannot simply be reduced to the number of deaths. A common symptom of COVID-19 is the appearance of ground glass opacities in chest X-rays, which indicate some sort of lesion. An autopsy carried out in Japan suggests that these opacities are damage to the alveoli, the pockets in the lungs where oxygen and carbon dioxide enter and leave the bloodstream. A study in China followed 90 COVID-19 patients (average age 45), who developed these lesions. Each individual was given several CT scans over a period of a month to track the progress of the lesions. While the extreme cases showed substantial recovery, the average degree of lung damage did not change significantly by the time the study ended. Moreover, of the 70 who were discharged, 94 percent still had lung abnormalities. [1]

A separate study of 58 asymptomatic individuals (average age 42) found that all had lesions in their lungs, despite the fact that only 16 went on to become outwardly sick. Of the 42 who did not go on to become clinically unwell, the lesions cleared up completely in half of them, while the rest showed some improvement.
For patients who do get better, recovery is seldom complete. In a study in Italy on patients who had been discharged from hospital, only 13 percent were free of all symptoms 60 days after they became unwell, and 44 percent reported a reduced quality of life. The main symptoms were fatigue, shortness of breath, joint pain, and chest pain. And we do not know how long the virus can remain in the body after recovery. Several individuals have recovered, and after multiple negative test results, suffered a relapse while still in quarantine and tested positive again. So the virus may remain for an indeterminate length of time, waiting to cause an opportunistic infection.
It is important to note that the virus does not just affect the lungs. Experiments on cell cultures have shown that the virus enters the cell via a membrane protein called ACE2, which can be found in the heart, intestine, kidney, and blood vessels as well as the lungs. And there is direct evidence that the coronavirus affects these organs; the Japanese autopsy showed blood clots in the kidney, which is a known cause of organ failure, as well as hemorrhages in the stomach and small intestine. And between 7 percent and 28 percent of hospitalized patients suffer an acute cardiac injury, while a third suffer from blood clots in the arteries or veins. If these clots block a vessel supplying the brain or lungs, it can result in serious complications or even death.
It’s well known that in acute cases, neurological side effects are caused by a so-called cytokine storm, where the body releases inflammatory agents in an uncontrolled manner in response to the infection. However, there are increasing reports of long COVID, which is not severe enough for hospitalization, but causes debilitating symptoms for weeks or months. The direct cause is unknown, as there is little evidence that the virus infects the nervous system, but it is now clear that neurological damage can occur even without a severe respiratory infection.
Neurological COVID-19 has not received enough attention, as hospitals are understandably occupied with the most acute cases. But a study of 43 patients in the United Kingdom shows how serious it can be. Many patients over 50 experienced strokes, caused by blood clots in a vessel supplying the brain. This age group was also susceptible to delirium and psychosis, although seven out of ten did recover. A small group of younger patients were hard to categorize, but symptoms included increased pressure in the skull, widespread microhemorrhaging, and a secondary bacterial infection in the brain.
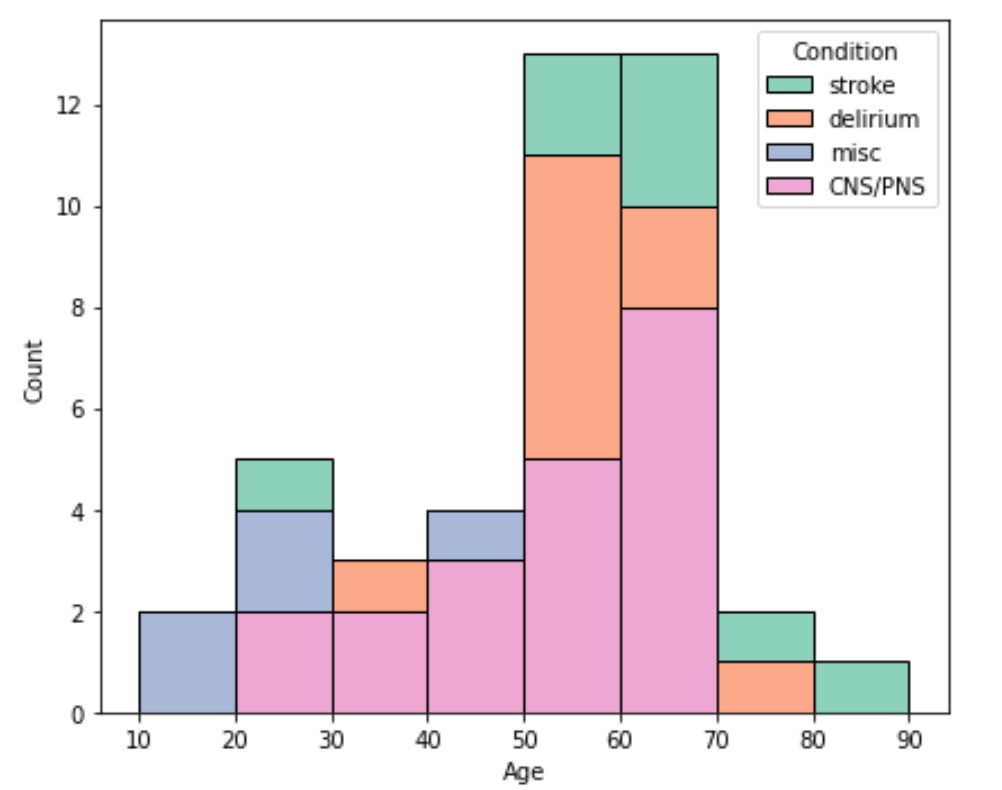
The most prevalent condition, affecting all ages, was measurable damage to the nervous system, presumably caused by an autoimmune response. Of the 43 patients, 12 had inflammations of the central nervous system (the brain and spinal cord). For the most part, this was damage to the protective covering surrounding nerve fibers, which could be seen as lesions or microhemorrhages using magnetic resonance imaging. These patients suffered from general weakness, fatigue and confusion, and had difficulty balancing. Seven patients had Guillain-Barré syndrome, an autoimmune condition where peripheral nerves lose their protective coating, which is diagnosed by measuring electrical activity in the muscles. The result is loss of sensation in the limbs and general weakness, which can progress to near paralysis. There is no known cure, and one in five people with Guillain-Barré syndrome are left with long-term problems.
It’s important to bear in mind that the above is a case study, so while it gives an indication of the most severe neurological symptoms, it does not represent the prevalence of such symptoms in the population as a whole. However, we can get some idea of the population statistics from TriNetX, who has been curating a database of 40,500 COVID-19 patients from around the world. Crucially, the database covers both inpatients (26 percent) and outpatients (74 percent), and has an even balance of individuals under and over 50.

Overall, 23 percent of the patients had neurological symptoms. Up to 2.7 percent had measurable neurological damage (stroke, movement disorders, peripheral nervous system damage, and nerve root disorders). The data confirm our general understanding of COVID-19: most people are not severely ill, but there’s a small chance of developing long-term effects including a debilitating neurological disorder. To put things in perspective, if everyone in the United States got COVID-19, we would expect up to 9 million individuals with such a disorder. The risk to the individual may be small, but at a population level, mass infection would be a public health catastrophe.
COVID-19 has been around for less than a year, so we don’t know how long its side effects will last. The 2002 SARS outbreak may give some indication of the prognosis for those requiring hospitalization, as it was caused by a similar (but more deadly) coronavirus. In 2017, survivors (average age 47) who had been hospitalized were far more likely to have developed chronic conditions than the population at large. Over half had metabolic disorders such as diabetes, 60 percent had developed osteonecrosis—a degenerative bone condition—and 44 percent had cardiovascular issues. Some of these conditions may have been caused by the corticosteroids used to treat patients, which are also being given to COVID-19 patients (including Donald Trump).

In a separate study on the long-term psychiatric effects of hospitalization, a quarter of SARS survivors were suffering from PTSD from their time in intensive care, while 16 percent were clinically depressed.
2. Those with the disease would have ‘died anyway’
Berenson cites Neil Ferguson—who originally trained as a theoretical physicist, but is now a professor of epidemiology at Imperial College, London—to claim that those who died were already on the brink of death:
More than half would likely have died within weeks or months in any case, as Neil Ferguson said in his British testimony. From any practical point of view, those deaths are unpreventable. Their timing is a function of the coronavirus, but their cause is underlying conditions such as cancer or heart disease or dementia.
Furthermore, Berenson cites a study that concluded that those admitted to care homes have very little time left to live:
A 2010 study in the Journal of the American Geriatrics Society found that half of all people admitted to nursing homes died within five months of admission (though the average length of stay was longer, because a fraction of residents lived several years after admission).
He also reports that a CBC investigation found that it is incredibly difficult to decide whether death is caused by an underlying condition or a more recent development:
Death can be complicated. If someone already extremely fragile with heart or lung disease is tipped over the edge with a flu infection, is that a flu death, or a heart death or a lung death? Which database gets to claim it?
Furthermore, Berenson cites a public health official as saying that anyone who tests positive for the coronavirus and subsequently dies, no matter the cause, will be counted as a COVID death:
If you were in hospice and had already been given a few weeks to live, and then you were also found to have COVID, that would be counted as a COVID death. It means technically even if you died of a clear alternate cause, but you had COVID at the same time, it’s still listed as a COVID death.
The implication is clear: so many of the fatalities were already terminally ill, and the criteria for assigning a COVID death are so lax, that the official COVID death figures are meaningless. Or in Berenson’s own words:
…the vast majority of people who die after becoming infected with coronavirus are old and unwell. In these cases, the distinction between dying WITH coronavirus as opposed to FROM coronavirus can be nearly impossible to make.
It sounds convincing, but does it hold up to closer inspection? While it is true that the combination of factors he gives could result in a distorted death count, he has not demonstrated that the death count has been distorted in this way. Berenson merely emphasizes the necessity of examining the evidence closely, giving this piece of advice gleaned from his years of investigative reporting: “If your mother says she loves you, check it out.”
So what do his sources actually say? The CBC report states that official mortality statistics for influenza are a gross underestimate, because autopsies are rarely performed. This also applies to suspected COVID-19 deaths, perhaps even more so because of the risk of infection to the doctors performing the autopsy. And what about Neil Ferguson, Berenson’s authority on this topic? What did he actually say in his statement to the British Parliament?
We don’t know what the level of excess deaths will be in the epidemic, in that, by the end of the year what proportion of people who died from Covid would have died [anyway]? It might be as much as half or two thirds of the deaths we see.
Even if we take Ferguson as a reliable source, all he is saying is that between zero and two thirds of the casualties maybe had less than a year to live, which is not a particularly strong claim. Yet we have actual data that shows that at this point in time, there have already been 275,000 more deaths in 2020 the United States compared to the baseline average from previous years, and this number is continually rising. Similar data for 23 European countries show 200,000 excess deaths, mainly individuals aged 45 and upwards.

And when it comes to the life expectancy of COVID fatalities, there has been an actual study: a team of researchers in Scotland has estimated that for coronavirus deaths in Italy, the average number of years of life lost is 13 for men and 11 for women. The researchers based this conclusion on the actuarial life expectancy of each individual, taking into account their age, gender, and the presence of long-term medical conditions.
Berenson is therefore making the claim that just by chance, several hundred thousand extra Europeans and Americans were about to die in April and March of this year, even if there had not been a pandemic.
While these facts do much to discredit Berenson’s argument that the coronavirus is not that bad, let’s look at his other major claim: that the experts have failed to manage the situation.

B. “The experts are incompetent: they cannot predict or solve the crisis”
1. “The models were wrong”
One of Berenson’s arguments centers on the Imperial College paper co-authored by Neil Ferguson, which we briefly mentioned earlier. Berenson summarizes the paper as follows:
…the report forecast 1.1 million Americans and 250,000 people in the United Kingdom could die even with months of efforts to reduce the damage. Only long-term “suppression” of society—possibly until a vaccine was invented—could lower those figures meaningfully, the researchers wrote.
This is a very fair summary of the paper. But Berenson then cites a report from The Daily Telegraph to claim that Ferguson subsequently changed his forecast to a much lower number:
British newspapers reported that Ferguson had dramatically changed his predictions. He now said his new best estimate was 20,000 Britons would die from the virus even with just weeks of quarantines.
Berenson clearly puts great stock in the new number:
For the second time in just over a week, I found myself stunned. Instead of 500,000 British deaths, 20,000? Without months or years of lockdowns? In the absence of a vaccine or effective treatment? … And, again, why hadn’t the New York Times and other American media outlets—after giving the earlier estimate so much attention—given equal prominence to the new number?”
Even if we take the claim that Ferguson changed his numbers at face value, what are we to conclude? If a forecaster changes a prediction by an order of magnitude, even though nothing material has changed, is it sensible to continue taking this person as an authority?
In the paper, Ferguson considers three situations in the United Kingdom:
- Up to 550,000 deaths in the unlikely event that the government takes no measures and individuals do not change their behavior.
- On the order of 250,000 deaths with a mitigation strategy of case isolation, household quarantine, and social distancing of the elderly.
- Between 5,600 and 120,000 with a suppression strategy using a combination of case isolation, home quarantine, social distancing, and school closure.
It is clear that Ferguson’s 550,000 figure was really just a baseline for a particular strategy, not a definitive prediction. As Ferguson said back on March 25:
“Fatalities are probably unlikely to exceed 20,000 with social distancing strategies but it could be substantially lower than that and that’s where real time analysis will be needed.”
The Daily Telegraph further clarified that:
Prof Ferguson said that the new social distancing measures announced by Boris Johnson earlier in the week meant the NHS would now be able to handle the incoming cases of coronavirus.
The measures announced that week were:
- A stay-at-home order.
- No public gatherings of more than two people.
- All non-essential services (gyms, churches, libraries…) to be closed.
As we can see, far from changing his prediction, Ferguson’s number of 20,000 deaths was in line with his forecast for a suppression strategy.
But that does not mean it was a good model in the first place. And this ties in with one of the critical questions that Berenson aims to answer in his book, namely:
“Why did the key predictive models that policymakers used when they agreed to lockdowns prove so inaccurate?”
Berenson is correct that the models were inaccurate—as of the time of this writing there have been more than 40,000 confirmed deaths in the United Kingdom, double Ferguson’s actual prediction—so I will endeavour to answer the question for him.
Modeling is common in science, but what is its aim? Usually, a model is a simplified representation of a physical system used to understand its fundamental properties. As long as the base assumptions are accurate, a model can give an indication of the qualitative properties of a pandemic, but it cannot accurately predict the number of cases or deaths. Every model has a number of tuneable parameters—such as the infection rate and the mortality rate—which are not known with great certainty. And this uncertainty can propagate and compound, rendering “prediction” very difficult with any accuracy.

To illustrate this point, the chart above shows the daily death rate in the United States, together with model predictions at the start of the pandemic and for the future. Despite an attempt to quantify uncertainty, one model underpredicted deaths in May by an order of magnitude. And future predictions differ so wildly that we could choose one to justify any policy we like.
Ferguson’s model was particularly poor in that it was too complicated to give any insight on the driving factors behind the pandemic. Rather than trying to build a simplified but informative description of reality, Ferguson had attempted to model every single individual, church, school, and office in the United Kingdom! Worse, the model had never been peer-reviewed beyond the vague description in the paper, and the program’s code was not available to the public. When the code was finally released in May, it took a team of professional software engineers several weeks to refactor it into a useable form.
So the real question is why was Ferguson, who has no formal training in public health, advising the British government? [2] And is Berenson simply focusing on Ferguson to undermine trust in public health officials?
COVID-19 is hardly the first pandemic in history, and the Centers for Disease Control and Prevention (CDC) in the United States have been studying pandemics for years. In fact, it’s literally their job! In 2007, they published a comprehensive plan for dealing with a future influenza pandemic. The report considered a novel respiratory infection with both asymptomatic transmission and a large number of asymptomatic cases. The plan had three major goals (with an overall aim of reducing the spread as much as possible while a vaccine was developed):
- Delay the exponential growth in the number of cases.
- Decrease the epidemic peak.
- Reduce the total number of cases.
The CDC knew very well that there would be a dearth of reliable information at the start of a pandemic, and that under such uncertainty the only course of action was to plan for the worst case scenario. For this reason, they developed a heuristic based on the case fatality ratio, which is the proportion of deaths among the already clinically unwell.
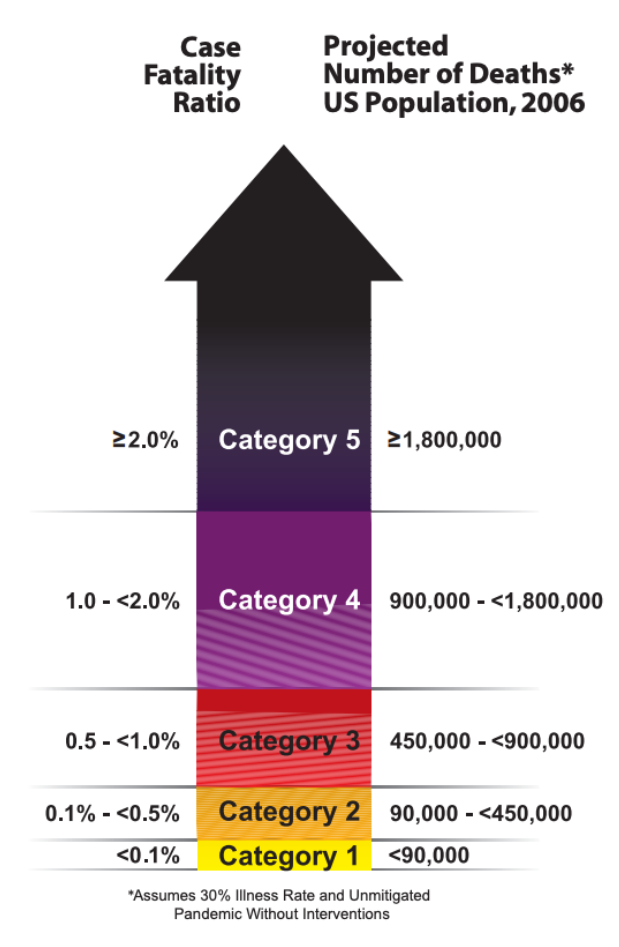
In January, the World Health Organization reported a case fatality ratio of 4 percent for COVID-19. By this metric, the United States should have started planning for a Category 5 pandemic immediately.
At that point in time, almost nothing was known about the virus. It could have been relatively minor, like the 2009 swine flu pandemic, or it could have killed a large portion of the world’s population, like the bubonic plague. This is not mere speculation—there is a branch of statistics called extreme value theory, which seeks to quantify the probability of extreme events. An analysis of historical pandemics shows that the only upper bound on the number of deaths is the human population of the earth. In the absence of good data, this is the worst case scenario.
The CDC’s recommendations are clear: action should have been taken as soon as community transmission had occurred on U.S. soil or in a city with strong transport links to the United States. The CDC recommended the following measures, with a planned duration of 12 weeks:
- Isolation of cases at home
- Quarantine of household members
- Closure of schools
- Social distancing
- Teleworking
- Cancellation of large public gatherings
The CDC knew from the 1918 pandemic that early adoption could drastically reduce the total number of deaths. But they also foresaw the present debacle:
The potential exists for such interventions to be implemented in an uncoordinated, untimely, and inconsistent manner that would impose economic and social costs similar to those imposed by strategically implemented interventions but with dramatically reduced effectiveness.
We can now return to Berenson’s argument. He may be mistaken on the science, and have little understanding of how to evaluate models and which models are worth evaluating in the first place, but we should give credit where credit is due if his practical suggestions are sound. What does he advocate that we actually do about the pandemic?
2. “Lockdowns do not work”
The term ‘lockdown’ refers to a government order to stay at home, combined with closure of transport and businesses. Berenson has stated several times that lockdowns do not work, and in his book he supports this claim by referring to an unnamed German research institute:
Still, real information continued to drip out—often tucked away in scientific papers that went unnoticed, such as when a German research institute reported in mid-April that lockdowns had been broadly useless.
I can find no such report, but I assume that he is referring to a comment made to the press by German virologist Hendrik Streeck:
I agreed with the initial restrictions and the ban on major events. After they were imposed, the infection process already started to decrease. I would have made further measures, such as contact restrictions, dependent on the actual course of the outbreak.
It’s not clear what Streeck meant by ‘initial restrictions.’ On March 13, all German states decided to close schools. Three days later, all states agreed on social contact restrictions—bars and clubs were closed, and shops had to restrict entry to prevent crowding. Germany’s death rate did not peak until mid-April.
Berenson also takes inspiration from China’s response to the coronavirus. He seems to think that China recovered from the pandemic largely without the help of lockdowns, and implies that we should use the same measures:
I found myself thinking of China. Not about what had happened in Wuhan, but about what hadn’t happened everywhere else. Shanghai and Beijing and other huge cities had avoided catastrophe. In early February, epidemiologists warned the Chinese lockdowns had come too late to matter. Instead, China was already tentatively reopening, restarting factories and dropping quarantines.
While Berenson is correct that China has fared better than the United States, this is because China was in fact quick to impose an incredibly strict lockdown. In early January, authorities in Wuhan reported an outbreak of an unknown type of pneumonia, and put all known close contacts under medical observation. Case numbers increased rapidly, and on January 23, the entire city was quarantined. Masks were made compulsory, large gatherings were cancelled, public transport was shut down, and all major routes in and out of the city were closed. Other cities in Hubei province passed the same measures in the following days. At this point in time, there had been only 650 confirmed cases in China. As the number continued to rise in February, the province began preventing residents from leaving their homes without permission, enforced by a team of 300,000 local officials.
Other major cities responded similarly. Shanghai enforced a 14-day quarantine on arrivals from Hubei on January 28, and placed checkpoints on its highways and travel hubs, where all travellers had their temperature recorded. Masks and temperature checks were enforced in public places, and by mid-February, officials were controlling access to private residences. Beijing imposed similar measures, and lockdowns were reintroduced whenever a new case appeared. Aggressive contact tracing, testing, and quarantines were used nationwide.
In comparison, the United States was slow to impose anything resembling the Chinese lockdown. In early March, citizens continued to enter the country from afflicted areas without being screened or quarantined. On March 12, when the United States had 1000 confirmed cases, President Trump banned entry for non-citizens arriving from Europe and China, but the measures taken internally were weak. In New York City—the worst-hit area—the subway remained open, and many left the city. Only five states (Alaska, Hawaii, Florida, Rhode Island and Texas) quarantined travellers from New York in late March, by which time New York State alone had over 7,000 confirmed cases. Checkpoints were only set up in August, and the city’s contact tracing program remained ineffectual.
In Europe and North America, lockdowns came too late to prevent widespread infection, but were they still a sound policy? This is a hard question to answer with complete certainty, as the infection rate and death rate took several weeks to stabilize in countries that imposed lockdowns. The best comparison we have is the difference in mortality between Norway, Denmark, and Sweden, which are broadly comparable in terms of demographics, health services, and climate. The major difference is that Norway and Denmark imposed strict lockdowns, while Sweden used much weaker voluntary measures.
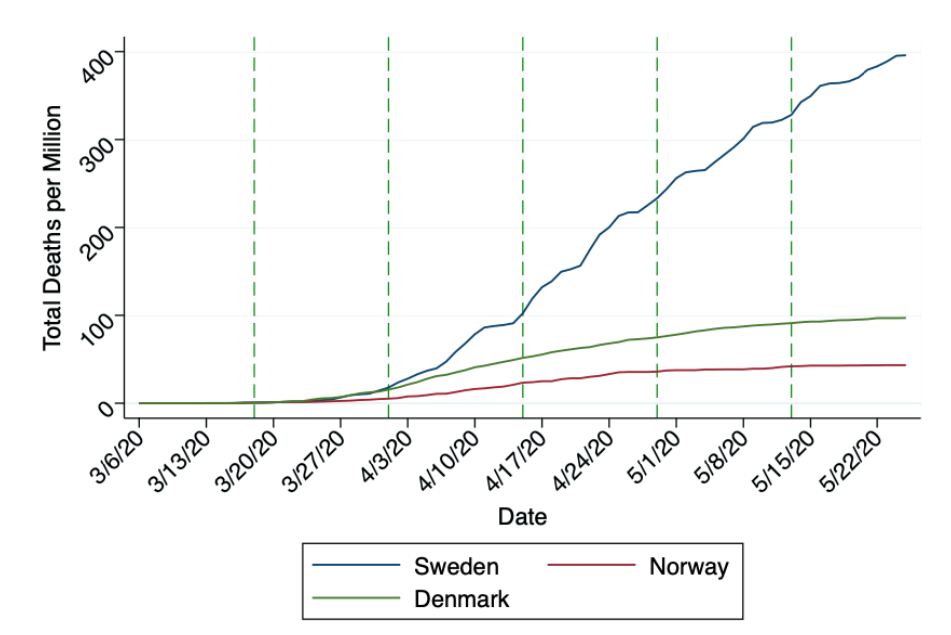
The numbers are stark: Sweden has suffered more than four times the number of COVID-19 deaths per million than Norway or Denmark.
Another favorite argument of Berenson’s against lockdowns is that the sunbelt states fared better than New York. In a Twitter post on July 31, he said the following:
AZ/FL/TX: 60 million people, no lockdowns (now), 23,000 peak hospitalizations, 500ish (hopefully) peak daily deaths.
New York: 20 million people, hard lockdown, 18,000 peak hospitalizations, 1000 peak daily deaths.
Let’s lockdown forever!
But this comparison is unfair. A statistical analysis of 50 cities worldwide suggests that climate plays a huge role in the spread of the coronavirus. Notably, areas with substantial transmission are located in the band of latitude 30° N to 50° N, with temperatures of 41° to 52° F (5° to 11° C). This almost exactly describes New York City in March.
What’s more, New York totally bungled its response to the coronavirus. Nursing homes were forced to take in sick patients, and the mayor of New York City famously urged citizens to go to the cinema mid-pandemic. A full lockdown was only enforced on March 22, when the state had already seen 15,000 cases and 118 deaths.
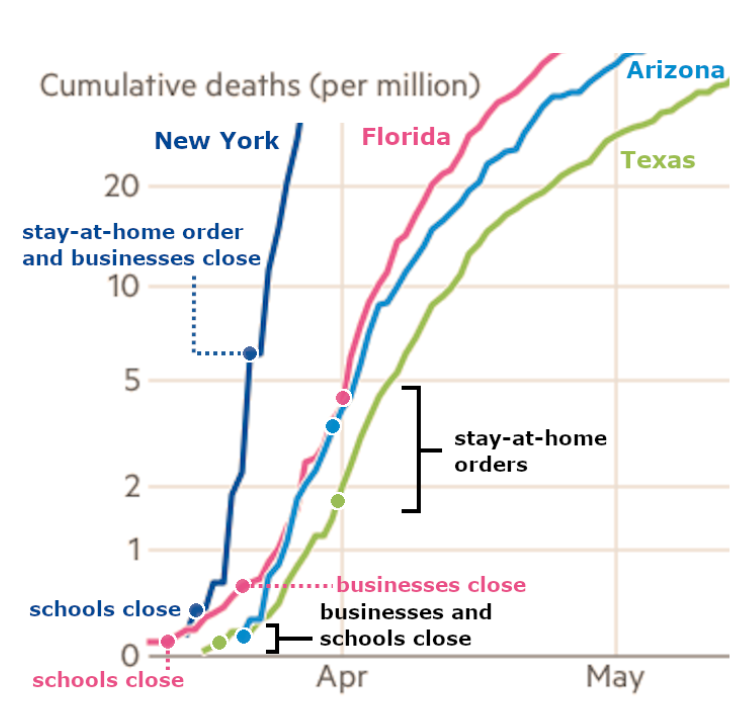
In comparison, the three sunbelt states started closing bars and restaurants well before the number of cases exploded, and when they did reluctantly lock down completely, their new case rate was far lower than New York’s when it imposed similar measures.
While the sunbelt lockdowns lasted, the number of deaths increased linearly, which indicates that the measures were working—if they hadn’t been working, the growth would have been exponential instead. However, all three states ended lockdown prematurely, and deaths started rising rapidly after a lag of approximately one month.

In the chart, the death rate does appear to be tapering off as of late September. The reason is not yet clear, but it could be due to the widespread adoption of masks.
Florida in particular has taken a high risk strategy. It has no statewide mask order, and its schools were recently forced to restart in-person teaching under threat of drastic budget cuts. The effect on the caseload remains to be seen.
3. “Lockdowns do more harm than good”
Berenson has started distancing himself from the claim that lockdowns don’t work at all, and has pivoted to saying that they do more harm than good. This is one of the main arguments in his book:
In less than three months, lockdowns have done incalculable damage. They need to be lifted as soon as possible. More importantly, we must agree that we will not restore them even if coronavirus deaths rise again in the fall and winter—unless hospitals face the real risk of collapse. The changes we have already made to protect the most vulnerable, as well as individual efforts at social distancing make a large wave of deaths less likely.
He does not provide evidence for this claim in his book—it entirely depends on whether you agree that we should just accept the deaths of the old and frail. However, he does elaborate on what he means by “incalculable damage” on his Twitter feed, where he claims that deaths caused by lockdown dwarf those caused by COVID-19:
The costs of lockdowns have been far higher than even the worst estimates (including their health costs; if #COVID deaths are overstated, lockdown deaths must be understates [sic]). Meanwhile their effectiveness appears to be near zero.
Again, to see the actual effect of lockdowns, we can return to Scandinavia, and this time compare excess deaths.

Sweden, without a strict lockdown, had far more excess deaths than either Norway or Denmark, which suggests that the number of lives saved by lockdown outstrips by far the number of lockdown-related deaths. And in terms of economic harm, Sweden fared little differently than its neighbors. In this light it’s misleading to consider lockdowns as the cause of economic harm—the pandemic causes enough economic damage by itself.
In another Twitter thread from mid-August, Berenson made perhaps his most dishonest use of statistics. He shared a chart from the U.S. Centers for Disease Control and Prevention, which compares weekly death counts from all causes based on age group.

Berenson said the following about this chart:
This age-stratified death data from @cdcgov is simple and compelling evidence about how much damage the lockdowns may have caused versus #Covid. Okay, first look at 85+ deaths.
…
Then deaths come almost back to normal (not quite, we know #Covid does cause excess deaths in the very elderly). By June they’re maybe 10-12% above normal. The Sunbelt spike brings them up to 20% above normal, 3,000 deaths a week or so, but still far below the April bump…
Okay, now look at deaths in the 25-44 range. They start to rise at the same time and rise almost as much. BUT THEY NEVER COME DOWN. They remain at 25-35% above normal every single week. We know these people are at exceptionally low risk from #Covid. THESE ARE LOCKDOWN DEATHS.
In short, he is arguing that lockdown causes 25-35 percent excess mortality in 25-44 year olds, while COVID-19 causes only 20 percent excess mortality in the very elderly. Therefore, he implies, lockdowns do more harm than good. This is misleading because the baseline number of deaths is, of course, much lower in 25-44 year olds. In terms of absolute numbers, the excess mortality for the younger group is about 1,200 in recent weeks, and 3,000 for the older group. But even if you accept the premises, the conclusion only follows if you assume a priori that lockdowns do not work. The only thing Berenson has shown is that there may be some lockdown-related deaths.
This is an important point. We should absolutely be concerned about the mental and physical effects of lockdown. Governments around the world have made a conscious choice on whether or not to support their citizens through the crisis. The U.S. government has been very willing to provide corporate bailouts, but has been much more reluctant to provide aid to individual citizens, or even cover the cost of medical treatment. With these priorities, suffering is inevitable.
4. “Masks do not work”
There is a possibility that the pandemic could be brought under control by widespread mask usage, even without lockdowns. There have been no good clinical trials on the effectiveness of masks, and it is unlikely that such a trial will ever take place—it would be unethical to require a cohort of doctors to forgo masks for the sake of the control group, and thereby risk both their own health and that of their patients. Such a trial was in fact attempted in China, but 37 percent of the doctors in the control group defied the study’s protocol and wore masks.
However, there is still good evidence that masks offer protection against viral transmission. In an Australian study, researchers had patients with clinically-confirmed influenza cough into a sample plate, with and without a mask. The samples were then analyzed for influenza RNA using the reverse-transcriptase polymerase chain reaction, which is a technique for replicating any viral RNA found in the sample until its concentration is above the detection limit. Influenza virus was detected in all of the plates from the control with no masks, but was not detected in the plates where patients had worn surgical masks or N95 masks. These findings are likely to apply to COVID-19 as well, as it has a comparable size (60-140 nm) to the influenza virus (80-120 nm). A similar study on a seasonal coronavirus came to the same conclusions.
Studies on the protective quality of masks for the wearer are more difficult, but have been carried out on mask-wearing mannequins set up to simulate human breathing. In one such study, the mannequin was sprayed with ultrafine salt particles (smaller than 200 nanometers) to mimic a virus. Under steady spraying, the surgical mask prevented 45 percent of the particles from entering the mannequin’s mouth. With explosive spraying 30 cm from the mannequin (to simulate coughs and sneezes), between 100 percent and 30 percent of the particles were blocked, depending on whether the mask was fully sealed or not. When the distance was increased to 60 cm, between 100 percent and 80 percent of the particles were blocked. This suggests that masks are highly effective at preventing transient transmission events, but are far less effective if spending extended periods of time in the presence of a sick individual. So if combined with social distancing, masks could largely prevent the spread of COVID-19.
However, we must examine the worst-case scenario, in which there are insufficient supplies of surgical and N95 masks, and the general public must make their own. A recent review of the literature suggests that homemade masks have an efficiency of zero to 50 percent at preventing outward viral spreading, while the inward protection efficiency is 20 percent to 80 percent. Taken together, these figures suggest that universal mask wearing could reduce the transmission rate by 20 percent if the homemade masks are all of poor quality, or by 90 percent if all the masks are high quality.
Given that Berenson is against lockdowns, are masks his solution to the pandemic? He says very little about masks in his book, but he shares his thoughts in a comment on Twitter, in response to the Surgeon General begging Fox News viewers to wear masks:
No, we’re going to take away your freedoms with mandatory isolation and quarantine orders and contact tracing; insisting you wear a mask is just a test of your willingness to accept pseudoscience and an effort to panic you.
And he explicitly says that masks are useless in a tweet on September 17:
Here’s the California report about the Spanish Flu I mentioned on @IngrahamAngle. Masks: useless in 1919, useless in 2020.
He includes a screen capture of a 1919 report from the California State Board of Health entitled The Wearing of Gauze Masks, with the following highlighted:
…the very complete records at the disposal of the California State Board of Health indicate conclusively that the compulsory wearing of masks does not affect the progress of the epidemic…
The evidence, the article explains, is that cities without compulsory masks fared the same or better than cities that made masks compulsory. However, the article specifies that the problem was the manner in which masks were used, not masks per se:
“…the masks were worn carefully under circumstances of least necessity, as upon the public streets and in the open air. They were just as conscientiously laid aside in private offices, and among gatherings of friends, the very places where the chances of contact with an early case of influenza and where the conditions for the transfer of droplet infection were the most favorable.”
It is also worth noting that the masks were made of gauze, which does not have a tight weave. We know the exact quality of 1918 gauze from a contemporary paper on surgical masks:
The gauze of which the masks were made varied in quality, some being as fine as twenty-eight strands to the warp and twenty-four to the woof per inch.
So the best gauze had only 52 threads per inch, while we know now that effective masks have at least 300 threads per inch.
5. “Herd immunity is the way to go”
So what is Berenson actually advocating? As we have seen, his book is more of a takedown than position paper, but in a New York Post article entitled “We could ‘beat’ COVID-19 before a vaccine is ready,” he comes close to endorsing the unproven strategy of herd immunity:
A growing number of scientists believe the threshold for herd immunity may be much lower. Some predict it might be 40 percent. Others say it could be as low as 20 percent—meaning that the epidemic will burn out after only 1 in 5 people is infected with and recovers from the virus.
…
If we can actually reach herd immunity after 40 percent or less of the population is infected, far fewer people will die than the early forecasts, even without lockdowns.
Herd immunity is a terrible idea for several reasons. Aside from the obvious public health disaster with mass fatalities, there is currently no proof that herd immunity is achievable. While there is encouraging evidence that the immune system produces antibodies and T cells in response to the coronavirus, we simply do not know how much protection these confer, or whether they will protect against all future strains. In the case of seasonal coronaviruses (which cause the common cold), it’s common for an individual to be infected twice by the same virus within a 12 month window. And there have been numerous reports of individuals getting COVID-19 twice, sometimes with increased severity.
Furthermore, a conscious strategy of trying to infect as many people as possible makes a second wave far more likely. A second wave can refer to two scenarios:
- Increase in infections and severity due to seasonal changes.
- A virus mutating into a more deadly strain.
The second possibility is particularly alarming. By advocating for herd immunity, Berenson is effectively advocating for a population scale virus incubator. The more people have the virus, the more likely it is to mutate into something much, much worse.
Post Mortem of a Berenson Argument
Berenson’s great flaw is over-optimism. His arguments always seem to hinge on the best-case scenario being true, yet he never convincingly demonstrates this to be the case. The most egregious example is when he simply assumes that the number of asymptomatic cases are equivalent to the hidden part of an iceberg, without quoting a single study:
For now, the crucial point is this: randomized antibody tests from all over the world have repeatedly shown many more people have been infected with coronavirus than is revealed by tests for active infection. Many people who are infected with SARS-COV-2 don’t even know it. So the hidden part of the iceberg is huge.
In the absence of a readily available test, we simply do not know the asymptomatic proportion. As of the time of this writing, the CDC gives a best estimate of 40 percent, with a lower bound of 10 percent and an upper bound of 70 percent. So Berenson might be right, but is it worth the risk? Who will take responsibility if we play Russian roulette with people’s lives and lose?
At times, Berenson borders on the conspiratorial; at others, he appears naïve. His astonishment that the media are “painting as bleak a picture of the coronavirus as possible” comes off as disingenuous, especially given that he originally made a name for himself by painting as bleak a picture as possible of marijuana. He portrays himself as a lone hero who dares to speak a truth that is being suppressed, but he rarely commits to a definite course of action, leaving himself room to deny what any reader would take as his obvious implications. His rhetorical technique is to signal his own credibility by listing errors (both real and imagined) made by journalists and scientists, but he provides little evidence to back up his claim that COVID-19 has largely ended as a medical crisis. His most cogent argument—that the current pandemic is not serious because the majority of deaths are among the elderly—is a question of morality, not science, and is repulsive to anyone who views the elderly as equal human beings. His claim that most case fatalities had only weeks or months to live is false.
It’s entirely possible that Berenson is sincere in his search for the truth about COVID-19, but his refusal to question his own premises will no doubt keep it far out of his reach.




